An international collaboration, featuring scientists from the University of Dundee, has made a breakthrough they hope will help futureproof a revolutionary new field of drug discovery by preventing resistance in cancer therapy.
An international collaboration, featuring scientists from the University of Dundee, has made a breakthrough they hope will help futureproof a revolutionary new field of drug discovery by preventing resistance in cancer therapy.
The latest developmental drugs used in oncology rely on the destruction of disease-causing proteins, rather than inhibiting their function as traditional therapies do. This targeted protein degradation is making the treatment of diseases previously thought to be undruggable a reality but, as with all drugs, there is the possibility of patients developing resistance to them.
In a study published today, researchers at CeMM, the Research Center for Molecular Medicine of the Austrian Academy of Sciences, and Dundee’s Centre for Targeted Protein Degradation (CeTPD) identify potential resistance mechanisms and provide insights on how to overcome them.
TPD drugs work like a glue by binding the defective, disease-causing protein to other proteins – known as E3 ligases – that switch on the body’s cellular waste disposal system. This then kick-starts the degradation process of the defective protein.
In their study, the authors identified a variety of mutations on E3 ligases which cause resistance in cell cultures. These include mutations already identified in patients whose therapy with degraders was unsuccessful.
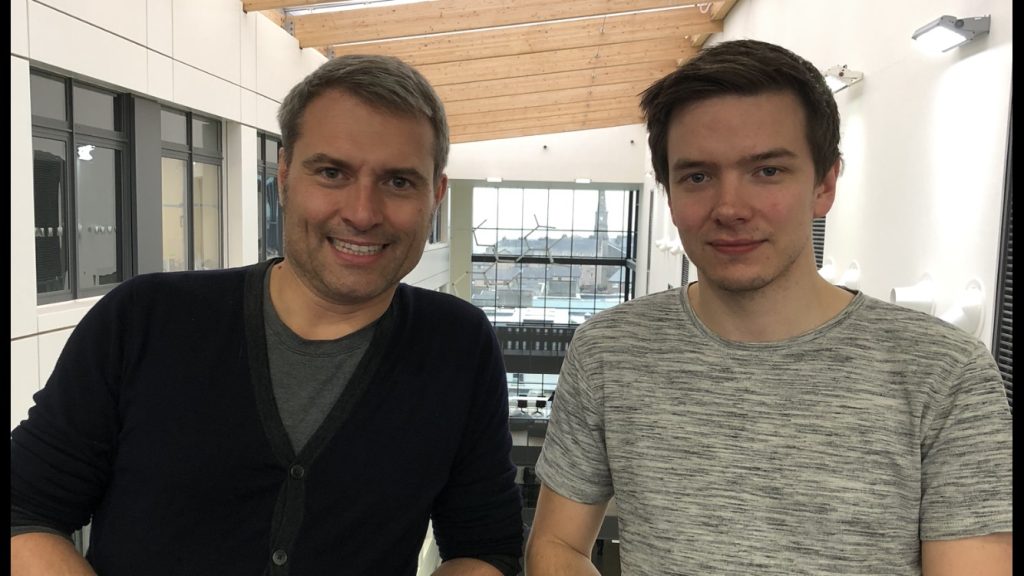
Ryan Casement, co-author and PhD student at CeTPD, led the biophysical structural work to investigate the resistance mutations and their molecular consequences to the degraders’ mode of action. He said, “A major finding of the paper is that key mutations arise in regions of the E3 ligase that come into close contact to the target protein.
“It was believed these degrader molecules worked by just bridging the two proteins across one another, but we now know that they actually form very intimate complexes, where the two proteins closely touch each other. Now we know that if a mutation arises in the region that is involved in such close interaction, then the patient can develop resistance to the drug.
CeTPD director Professor Alessio Ciulli said, “For the first time we have been able to examine at the molecular level how drug resistance emerges by virtue of these E3 ligase mutations. This is extremely important because these findings highlight the mechanism that can anticipate how a patient might respond to these drugs.
“Stopping mutations from forming completely is going to be very challenging but we can think about how to delay them by designing treatment differently. Armed with the knowledge that these mutations are likely or have a potential to arise, we can also think ahead to second-generation drugs that could still be active with this mutational background.”
A number of degrader drugs are currently being tested in clinical trials, while some are already available to patients, especially for various types of blood cancers.
The study, published today in Nature Chemical Biology, is anticipated to make an important contribution to the improved design of degraders. Cancer patients, in particular, could benefit from a clinical application of the findings in the future.
Both the University of Dundee and CeMM are world leaders in the study of targeted protein degradation, which is applicable to diverse therapeutic areas including inflammation, dermatology, immunology, and respiratory diseases as well as oncology.
Georg Winter, Principal Investigator at CeMM, said, “We tested a large number of different proteins and degraders. On one hand, we see that some mutations in E3 ligases prevent defective proteins from being recruited. At the same time, however, we see that some of these mutations exhibit high sensitivity to chemically modified degraders.
“Therefore, mutations can still be targeted by changing the chemical structure of the degrader. In other words, resistances can be overcome.”
Read the story on:
