EDUCATION
What is Bronchiectasis?
Bronchiectasis is a common, progressive lung condition where the large- and medium-sized airways become abnormally widened and accumulate large volumes of thick mucus which lines and clogs the airway.
As such, those with bronchiectasis often present with symptoms including chronic cough, breathing difficulty and an increased susceptibility to severe chest infections, although symptoms are highly heterogeneous – meaning the symptoms patients experience, and the severity of these symptoms, can vary between individuals.
Periodic flare ups of symptoms are referred to as ‘exacerbations’ and not only worsen patient quality of life, but are a main driver of bronchiectasis disease progression, severity, morbidity and (in severe cases) mortality.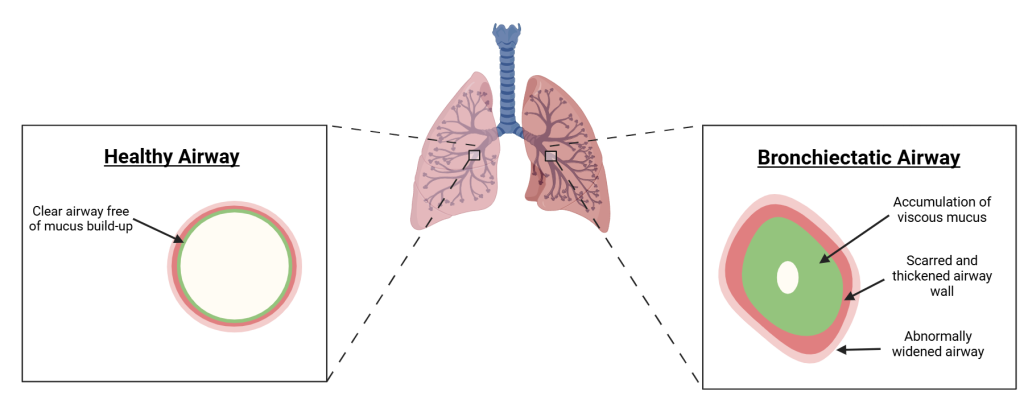
What causes bronchiectasis?
There are multiple known causes of bronchiectasis, but it most commonly arises following respiratory infection, particularly severe infections that occur repeatedly during childhood.
Bronchiectasis can also be a consequence of various genetic conditions (such as Primary Ciliary Dyskinesia and Alpha-1 Anti-Trypsin Deficiency), inherited or acquired immunodeficiencies, other respiratory conditions (such as asthma and Chronic Obstructive Pulmonary Disease) and/or systemic inflammatory conditions (such as inflammatory bowel disease and rheumatoid arthritis).
However, the majority of individuals with bronchiectasis have ‘idiopathic bronchiectasis’, meaning their bronchiectasis has no identifiable cause.
Bronchiectasis is said to develop as a result of a complex, self-sustaining cycle of chronic inflammation, infection, impaired mucus clearance and structural lung damage – often referred to as a ‘vicious vortex’.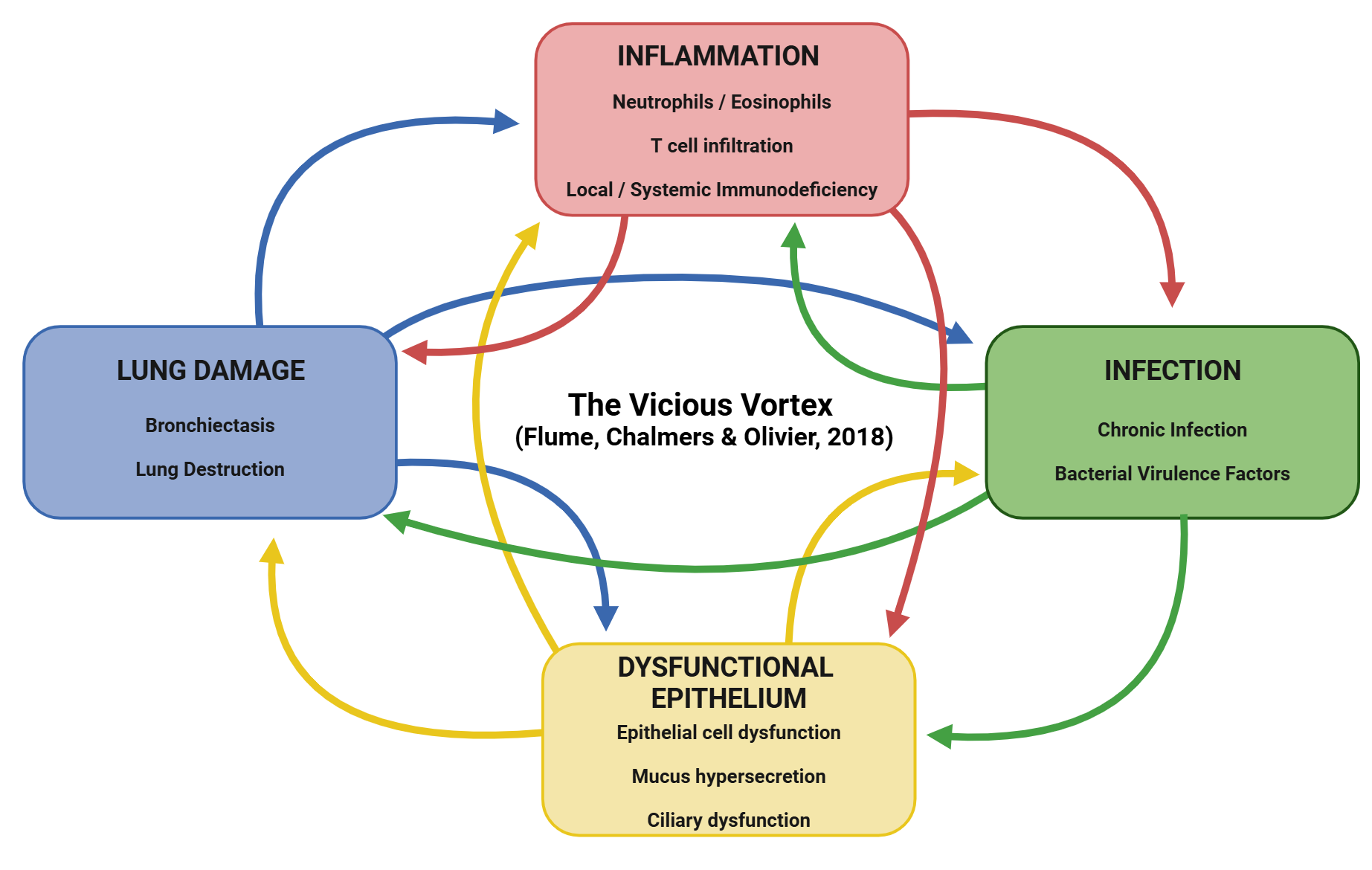
How do you treat bronchiectasis?
 While there is currently no cure for bronchiectasis, mainstay treatments aim to alleviate symptoms, reduce exacerbations, prevent disease progression and improve patient QoL, mainly by tackling chronic infections and improving mucus clearance.
While there is currently no cure for bronchiectasis, mainstay treatments aim to alleviate symptoms, reduce exacerbations, prevent disease progression and improve patient QoL, mainly by tackling chronic infections and improving mucus clearance.
With growing evidence showing that inflammation is a key component of the processes driving bronchiectasis development and progression, much research is being conducted to determine the clinical benefit of anti-inflammatory therapies in bronchiectasis.
Examples of treatments currently recommended for use in bronchiectasis – according to current treatment guidelines – are shown below.
For full guidance regarding the management of bronchiectasis, please consult the ERS Bronchiectasis Treatment Guidelines.
Treatment | Examples | Rationale for Use |
Antibiotics (oral) | Penicillins, Tetracyclines Macrolides (low dose) | To treat / prevent chronic bacterial infections To elicit broad-spectrum immunomodulatory / anti-inflammatory effects |
Antibiotics (inhaled) | Tobramycin, colistin | To treat / prevent chronic bacterial infections |
Bronchodilators | Beta 2-adrenergic agonist, long-acting muscarinic antagonists (LAMA) | To relax airway smooth muscle, open airways and improve breathing. |
Immunisations | Vaccination against seasonal Influenza, pneumococcal, COVID etc | To prevent respiratory infections triggering exacerbations. |
Inhaled corticosteroids (ICS) | Budesonide, fluticasone | To reduce airway inflammation in those with respiratory comorbidities (i.e., asthma and/or COPD) |
Mucoactive Drugs | Nebulised hypertonic saline solution, isotonic saline, Guaifenesin, Mannitol, oral N-acetylcysteine, oral carbocisteine | To regulate mucus secretion and alter mucus viscosity, promoting mucus clearance from the airways |
Airway Clearance Techniques | Active Cycle of Breathing Techniques, autogenic drainage, postural drainage alongside percussion, vibration, huffing and coughing | To aid removal of mucus from the airways. |
Mucus Clearance Devices | The Flutter, the RC cornet, the Acapella | To aid mucus clearance from the airways by vibrating/dislodging mucus. |
Pulmonary Rehabilitation | Exercise, education, and support | To improve breathing problems. |
Surgery | Lobectomy/pneumonectomy | To remove the affected lobe/section of the lung. |
Educational Resources on Bronchiectasis
To learn more about bronchiectasis, we encourage you to visit the following resources:
For patients:
Bronchiectasis in Adults: resources provided by Asthma+Lung UK – resources cover what bronchiectasis is, what the symptoms are, and how it is diagnosed and treated.
Bronchiectasis in Adults: resources provided by the European Lung Foundation – resources cover what bronchiectasis is, what the symptoms are, and how it is diagnosed and treated, with additional online resources for patients.
Also see our ‘Patient Partners & Resources’ page for more patient-friendly resources on bronchiectasis.
For clinicians and industry:
Bronchiectasis: a neglected and overlooked lung condition with unrealised commercial potential – LifeArc – a campaign issued by LifeArc in collaboration with industry experts and and Asthma+Lung UK to raise awareness and support the advancement of new innovations and research into bronchiectasis
Bronchiectasis | Health topics A to Z | CKS | NICE – medical information including disease background, diagnostics and disease management/prescribing information.
For respiratory professionals (clinicians, scientists etc):
Basic, Translation and Clinical Aspects of Bronchiectasis in Adults (Chalmers, Elborn & Greene., 2023) – a review article discussing the processes underpinning the development and proigression of bronchiectasis.
Rethinking bronchiectasis as an inflammatory disease – The Lancet Respiratory Medicine – a review article detailing bronchiectasis as an inflammatory disease and the concept of disease activity versus disease severity.
We also encourage clinicians and respiratory professionals to browse the educational resources ‘For Respiratory Professionals‘ to learn more about key topics related to bronchiectasis.
We encourage primary care physicians to browse the educational resources ‘For General Practitioners‘ to learn more about the diagnosis and management of bronchiectasis.
Have ideas for educational resources on bronchiectasis?

If you have ideas for educational content, courses or webinars that you would like EMBARC to provide, please email your suggestions to contact@bronchiectasis.net.
